Eye Diseases
Refractive error
A refractive error is the second major cause of visual impairment. Despite that it can be corrected simply by a pair of spectacles, millions remain blind or visually impaired due to uncorrected refractive error.
Uncorrected refractive error remains largely unaddressed – this is contributed to by a complicated web of barriers.
The cornea and lens of your eye helps you focus. Refractive errors are vision problems that happen when the shape of the eye keeps you from focusing well. The cause could be the length of the eyeball (longer or shorter), changes in the shape of the cornea, or aging of the lens.
Four common refractive errors are
The most common symptom is blurred vision. Other symptoms may include double vision, haziness, glare or halos around bright lights, squinting, headaches, or eye strain.
Glasses or contact lenses can usually correct refractive errors. Laser eye surgery may also be a possibility.
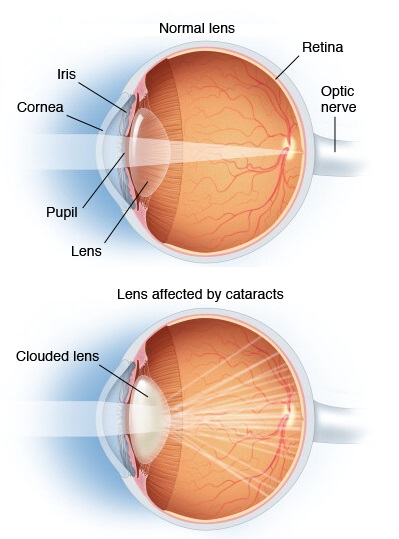
Cataract
What is Cataract?
A cataract is a clouding of the lens in the eye that affects vision. Most cataracts are related to aging. Cataracts are very common in older people. By age 80, more than half of all Americans either have a cataract or have had cataract surgery.
A cataract can occur in either or both eyes. It cannot spread from one eye to the other.
What are the symptoms of a cataract?
The most common symptoms of a cataract are:
How is a cataract detected?
Cataract is detected through a comprehensive eye exam that
1.) Visual acuity test - This eye chart test measures how well you see at various
2.) Dilated eye exam - Drops are placed in your eyes to widen, or dilate, the pupils. Your eye care professional uses a special magnifying lens to examine your retina and optic nerve for signs of damage and other eye problems. After the exam, your close-up vision may remain blurred for several
3.) Tonometry - An instrument measures the pressure inside the eye. Numbing drops may be applied to your eye for this
Your eye care professional also may do other tests to learn more about the structure and health of your
Keratoconus
What is Keratoconus?
Keratoconus is a condition of the eye in which the structure of the cornea (the clear outer part of the eye) is not strong enough to hold its round shape, causing it to bulge outwards like a cone.
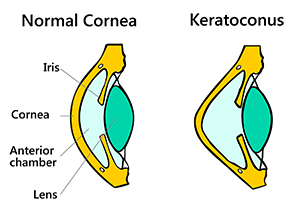
Often, this condition is hereditary and occurs more frequently in people with certain medical problems.
Progression of the outward corneal bulging can happen very quickly or can occur over several years, though these changes can stop at any time.
How Will Keratoconus Affect My Vision?
Keratoconus will change vision in two ways:

Symptoms
Retinal Detachment
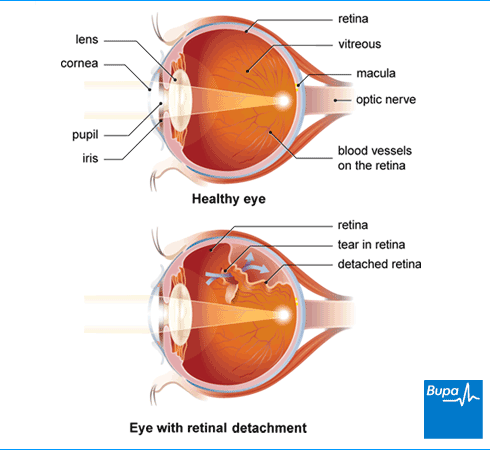
What is Retinal Detachment?
The retina is a thin, light-sensitive tissue that covers the inside back portion of the eye. In most cases retinal detachment is caused by the presence of one or more small holes or tears in the retina.
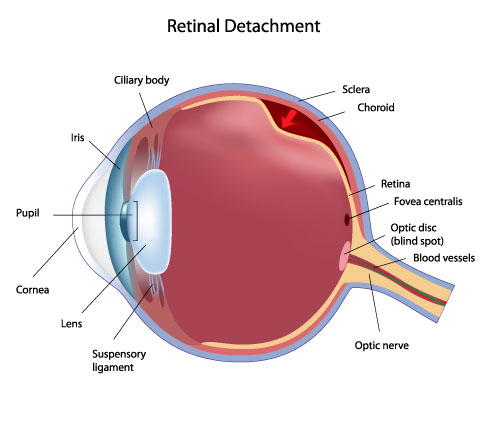
When a retinal tear is present, watery fluid from the vitreous space may pass through the hole and flow between the retina and the back wall of the eye. This separates the retina from the back of the eye and causes it to detach. The detached portion of the retina will not work properly, and there will be a blur or
blind spot in the vision.
Types of Retinal Detachment
Rhegmatogenous retinal detachment - a break, tear or hole develops in the retina, allowing liquid to pass from the vitreous space into the subretinal space between the sensory retina and the retinal pigment epithelium (the pigmented cell layer just outside the neurosensory retina).
Secondary retinal detachment - also known as exudative retinal detachment or serous retinal detachment. It is caused by inflammation, vascular abnormalities or injury which cause fluid to build up under the retina (there is no hole, break or tear).
Tractional retinal detachment - an injury, inflammation or neovascularization causes the fibrovascular tissue to pull the sensory retina from the retinal pigment epithelium.
What are the signs and symptoms of a detached retina?
Photopsia - the patient experiences sudden flashes of light which are very brief and in the outside of center part of their vision (peripheral vision). The flashes more commonly occur when the eye moves.
An enormous increase in the number of floaters. Floaters are bits of debris in the eye which make us see things floating in front of us, usually like little strings of transparent bubbles or rods that follow our field of vision as our eyes turn. Often it may be a ring of hairs or floaters on the temporal side of the central vision
The eye feels somewhat heavy
A shadow starts to appear in the peripheral vision. It gradually spreads towards the center of the person's field of vision
A sensation that a transparent curtain is coming down over the field of vision
Straight lines start to appear curved
Treatment
There are several methods of treating a detached retina, each of which depends on finding and closing the breaks that have formed in the retina. All three of the procedures follow the same three general principles:
Scleral buckle surgery
Scleral buckle surgery is an established treatment in which the eye surgeon sews one or more silicone bands (bands, tyres) to the sclera (the white outer coat of the eyeball). The bands push the wall of the eye inward against the retinal hole, closing the break or reducing fluid flow through it and reducing the effect of vitreous traction thereby allowing the retina to re-attach. Cryotherapy (freezing) is applied around retinal breaks prior to placing the buckle. Often subretinal fluid is drained as part of the buckling procedure. The buckle remains in situ.
The most common side effect of a scleral operation is myopic shift. That is, the operated eye will be more short sighted after the operation. Radial scleral buckle is indicated for U-shaped tears or Fishmouth tears, and posterior breaks. Circumferential scleral buckle is indicated for multiple breaks, anterior breaks and wide breaks. Encircling buckles are indicated for breaks covering more than 2 quadrants of retinal area, lattice degeneration located on more than 2 quadrant of retinal area, undetectable breaks, and proliferative vitreous retinopathy.
Pneumatic retinopexy
This operation is generally performed in the doctor's office under local anesthesia. It is another method of repairing a retinal detachment in which a gas bubble (SF6 or C3F8gas) is injected into the eye after which laser or freezing treatment is applied to the retinal hole. The patient's head is then positioned so that the bubble rests against the retinal hole.
Patients may have to keep their heads tilted for several days to keep the gas bubble in contact with the retinal hole. The surface tension of the gas/water interface seals the hole in the retina, and allows the retinal pigment epithelium to pump the subretinal space dry and "suck the retina back into place". This strict positioning requirement makes the treatment of the retinal holes and detachments that occurs in the lower part of the eyeball impractical. This procedure is usually combined with cryopexy or laser photocoagulation.
Pneumatic retinopexy has significantly lower success rates compared to scleral buckle surgery and vitrectomy. Some initially successful cases will fail during the weeks and months after surgery. In some of the failed cases, an area of the retina which was healthy and attached prior to the initial pneumatic retinopexy repair procedure develops new tears and/or becomes detached.
Vitrectomy
Vitrectomy is an increasingly used treatment for retinal detachment. It involves the removal of the vitreous gel and is usually combined with filling the eye with either a gas bubble (SF6 or C3F8 gas) or silicone oil. An advantage of using gas in this operation is that there is no myopic shift after the operation and gas is absorbed within a few weeks. Silicon oil (PDMS), if filled needs to be removed after a period of 2–8 months depending on surgeon’s preference.
Silicone oil is more commonly used in cases associated with proliferative vitreo-retinopathy (PVR). A disadvantage is that a vitrectomy always leads to more rapid progression of a cataract in the operated eye. In many places vitrectomy is the most commonly performed operation for the treatment of retinal detachment.
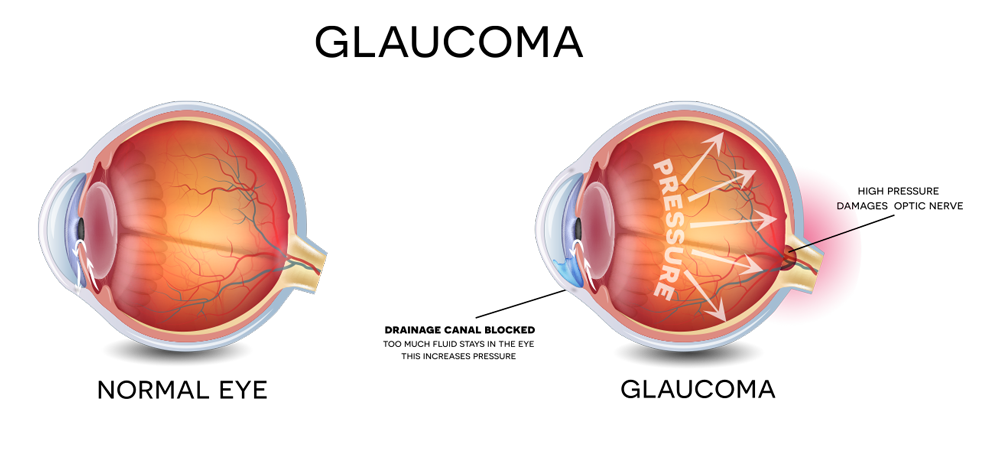
Glaucoma leads to severe consequences like blindness or permanent change in vision, if ignored or goes untreated. It’s a disease which happens due to damage of the optic nerve from excess fluid pressure in the eye, which is also known as aqueous humour. Latest treatment methods suggest anti-glaucoma compositions that are effective in reducing the intraocular pressures.
Squint
What is Squint?
Intermittent or constant, this deficiency takes place because eyes get misaligned, in different directions. Usually, the eyes are supported and held by 6muscles, but in case of squint, the stronger muscle pulls the eye towards it, and it can be inward or outward. The reasons can be varied, like heredity, nerves defect, poor vision or defect of eye muscles. This disorder can happen at any age, but empirically, studies have cited, they happen in infants and young children.

Adjustable Suture Strabismus Surgery
With adjustable suture eye muscle surgery, your surgeon adjusts sutures holding eye muscles in place after a resection procedure, to attempt to improve your final outcome.
Strabismus surgery corrects alignment of the eye muscles.
Generally this surgery is possible only in adults, with perhaps only a small percentage able to benefit. This surgery is probably best for someone in whom strabismus developed in adulthood after previously normal eye alignment. In this case, the person is a good candidate because of fusion potential — the ability of both eyes to "lock on" to a target simultaneously, resulting in stereovision and a high degree of depth perception.
In this case, the person is a good candidate because of fusion potential — the ability of both eyes to "lock on" to a target simultaneously, resulting in stereovision and a high degree of depth perception. In most cases, adjustable suture surgery is performed in the operating room, with general or local anesthesia. Afterward the eye is patched. About four to 24 hours later, the patch is removed in the office, when anesthesia and sedation have faded. Ocular alignment is then evaluated.
Based on how your eyes are aligned, your surgeon may decide to use the suture that is in place to tighten or loosen the treated muscle. This adjustment may cause slight discomfort, primarily with muscle tightening. Once the desired alignment is achieved, the surgeon ties the adjustable suture permanently in place, and the procedure is complete.
Diabetic Retinopathy
What is Diabetic Retinopathy
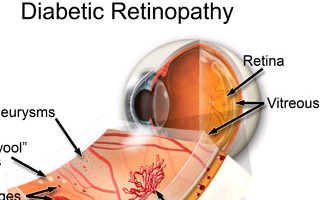
Diabetic retinopathy is the most common among the diabetic eye disease. It is caused by changes in the blood vessels of the retina. All persons with diabetes - both type 1 and type 2 - are at risk. That's why everyone with diabetes should get a complete dilated eye test done at least once a year.
Age Related Macular Degeneration
What is Age Related Macular Degeneration?

Age-related macular degeneration (AMD) is a breakdown of your eye's macula. The macula is a small area in your retina — the light-sensitive tissue at the back of the eye. This macula is responsible for your central vision, allowing you to see fine details clearly.There are two types of macular degeneration - wet and dry.
Blocked Tear Duct
What is Blocked Tear Duct?
The main objective of carrying out the Dacryocysorhinostomy (DCR) Surgery is to relieve the sticky, watery eye which is caused by tear ducts (nasolacrimal duct) blockage that is between the lacrimal sac or tear sac that is at the extreme corner and the outflow gap or passage of the tear into the back of the nose.
Causes Of blocked tear duct
Causes of blocked tear ducts in children include:

Blocked tear ducts may run in families. In adults, blocked tear ducts may be caused by an injury to the bones or tissues around the eyes or by another disorder, sometimes related to aging. For example, a blocked tear duct may result from a thickening of the tear duct lining, abnormal tissue or structures in the nose, or problems from surgery on or around the nose.
Symptoms Of blocked tear duct
Symptoms often affect only one eye. They may include:
Babies who have blocked tear ducts usually have symptoms within the first few days to the first few weeks after birth.
The symptoms of a blocked tear duct may get worse after an upper respiratory infection, such as a cold or sinus infection. Wind, cold, and sunlight also may make symptoms worse.
How is a blocked tear duct diagnosed?
A blocked tear duct is diagnosed based on a medical history and a physical exam. The doctor may also use tests to measure the amount of tears or to see if tears are draining normally from the eyes. Other tests can help your doctor find out where the blockage is or how it was caused.
Low Vision and Visual Rehabilitation
What is Low Vision and Visual Rehabilitation?
Integrating medical, educational, and rehabilitative services in the treatment of low vision

The Low Vision and Visual Rehabilitation Service can help individuals with all levels of vision loss ranging from mild visual impairment to legal blindness. Our comprehensive, multi-disciplinary approach to care provides a team of specialists — from ophthalmologists to optometrists to occupational therapists —who are trained to evaluate your condition and identify an individualized rehabilitation plan to help you maximize remaining functional vision and maintain independence in daily living.
What is low vision?
Nearly 14 million Americans have low vision — a condition characterized by a level of vision that is 20/70 or worse and that cannot be fully corrected with medical treatment, surgery, or conventional glasses. Unlike total blindness, most individuals with low vision have some useful sight. But, as vision deteriorates, those affected often find it difficult to accomplish the tasks of everyday life — such as reading, recognizing faces, cooking, driving, and differentiating color.
Low vision can occur at any stage in life, but it primarily affects the elderly. Most people develop low vision as a result of eye conditions and diseases, including macular degeneration, diabetic retinopathy, glaucoma, cataracts, retinitis pigmentosa, and stroke. Some causes of low vision, such as cataracts, are treatable and good vision can be restored. When diagnosed early, other conditions that lead to low vision, such as wet macular degeneration and glaucoma, can be halted or slowed — although vision lost is irreversible.
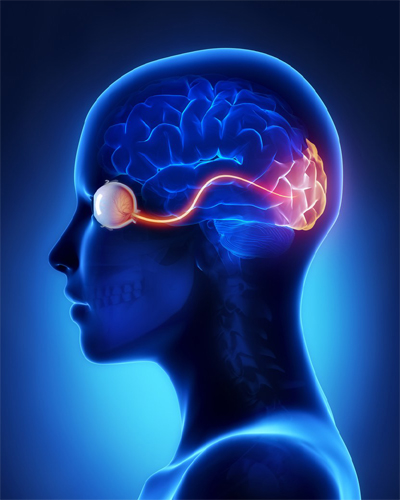
Neuro Ophthalmology
What is Neuro Ophthalmology?
Neuro-ophthalmology is the branch of Ophthalmology that deals with diseases of the eye in relation to the nervous system. These fall into two main groups:

Optic Nerve Diseases
What is Optic Nerve Diseases?
The optic nerve is the only nerve in the body that can be directly examined by a doctor. It connects the eye to the brain. The optic nerve can be affected by:
Orbit Oculoplasty& Ocular Oncology
What is Orbit Oculoplasty& Ocular Oncology?
Orbit, Oculoplasty and Ocular Oncology, a distinct subspecialty handles anomalies of lids, lacrimal system, extra ocular structures, bony orbit and other ocular adnexa. The orbit clinic receives a number of referrals of case of common and uncommon orbital tumors, orbital inflammations and infections which are managed both conservatively with medical management, chemotherapy and surgically with the removal of the tumor via orbitotomy. A large number of patients with thyroid related orbitopathy are treated (in collaboration with the general physician) on a daily basis. Naso lacrimal duct obstructions both congenital and acquired are routinely treated by us, with probing, external/ endonasaldacryocystorhinostomy, Jones' tube placement and ballondacryoplasty. Orbital floor fracture repair with implants (silicon, prolene mesh and medpor) are commonly done. Aravinds Orbit and Oculoplasty services are available at Aravind Madurai, Tirunelveli, Coimbatore and Pondicherry.

A number of patients are seen in the Oculoplasty clinic daily with a variety of eyelid disorders including malpositions (Ptosis, entropion, ectropion), benign and malignant eyelid tumors, facial dystonias etc. Surgical corrections for ptosis, entropion, ectropion, eyelid reconstructions post tumor removal as well as number of cosmetic eyelid surgeries (e.g. Blepharoplasty) and injection of botulinum toxin (Botox) for facial dystonias and cosmetic indications are performed.
The ocular oncology unit, now a referral centre administers chemotherapy for the relatively common retinoblastoma, and other rarer ocular cancers. Chemotherapy sessions are administered at Aravind, in consultation with a local oncologist. A trained nurse attends to their needs while an experienced medical officer stops by for regular check-ups.
Pedratric ophthalmology
What is Pedratric ophthalmology?
Even when vision problems are just one part of a complex health condition, ophthalmology in children is part of helping kids reach their full potential.

From the youngest children who can’t tell us what they see, to those getting their first pair of glasses, we focus on the unique eye care needs of kids. Our pediatric ophthalmologists help your child achieve the best vision possible with routine and specialized care such as:
About Uvea Clinic
The clinic caters to patient with different types of uveitis and other related types of inflammation of eye and adjoining tissues.
Getting to know uveitis
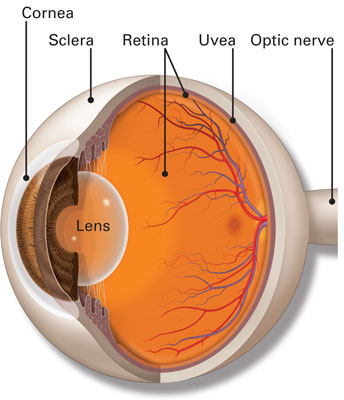
The uvea is the middle layer of the wall of the eye. It has three parts: the iris, the ciliary body and the choroid. Inflammation (or swelling) of any part of the uvea is termed "uveitis." Uveitis can be classified by the area where the inflammation appears.
If the primary area involved is the iris, the condition is called "iritis";"cyclitis" if on the ciliary body and "choroiditis" if on the choroid. Uveal inflammation may also spread to adjacent tissues. For example, choroiditis may spread to the retina and thus becomes a "chorioretinitis."
The symptoms of uveitis depend upon the area that is inflamed and the duration of inflammation. Acute iritis may cause a red eye with pain and sensitivity to light. Chronic and posterior inflammation may be painless but may cause symptoms such as floaters or decreased vision.